How Rheumatoid Arthritis affects the Lungs?
Rheumatoid arthritis (RA) is a well-characterized, progressive autoimmune disease that primarily affects the joints through various mechanisms, including inflammation, pain, and ultimately damage to bone and cartilage.
But remember, RA is a systemic disease; it affects other parts of the body as well, and that includes the lungs. Indeed, pulmonary complications are one of the most severe extra-articular manifestations of RA and represent a major cause of morbidity and mortality among patients with the disease [1].
The Connection Between Rheumatoid Arthritis and Lung Disease
This is because RA is a chronic autoimmune disease that affects the lungs. Not only does RA inflammation trigger in joints, but it also leads inflammation to other tissues as well, such as lungs [9]. The immune system mistakenly attacks the body’s own cells, causing chronic inflammation and damage to lung tissue. This damage can manifest as varying injury to some parts of the respiratory system, such as the airways, lung tissue, or pleurae.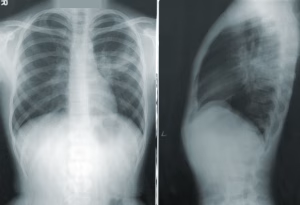
The relative probability of lung involvement in RA is affected by disease severity (attributable to illness activity, treatment status, and comorbidities), smoking history, environmental exposures, and genetic predisposition.
Q1. What lung complications can occur in association with rheumatoid arthritis?
Rheumatoid lung disease [RLD] is not a single clinical entity but rather a very heterogeneous group of pulmonary disorders associated with RA, each with its own unique diagnostic and therapeutic challenges.
Interstitial Lung Disease[ILD]
Interstitial lung disease (ILD) is one of the most undiagnosed lung complications associated with RA. It can affect the lungs and cause scarring (the formation of fibrous tissue) that can limit the lungs’ functioning by transferring oxygen into the circulatory system. Symptoms of ILD include:
Persistent dry cough
— Dyspnea, especially with exertion
Fatigue
The severity of ILD spans from mild to severe and can occasionally have an aggressive course, resulting in respiratory failure. Rheumatoid arthritis-associated ILD (RA-ILD) may be particularly difficult to treat and can substantially impair quality of life.
Pleural Disease
Rheumatoid arthritis (RA) can also influence the pleura, thin membranes enclosing the lungs. Pleural disease can occur as pleuritis, which means inflammation of the pleura, or as pleural effusion (accumulation of fluid between layers of the pleura).
Chest pain — particularly when taking a deep breath Sudden and severe difficulty breathing due to fluid accumulation Although pleural disease occurs less frequently than ILD, it can still cause significant morbidity if not effectively treated.
Nodules in the Lungs
Rheumatoid nodules are non-cancerous lumps that can develop in the lungs of people with RA. These nodules are typically asymptomatic and found incidentally on imaging studies; however, larger nodules may cause cough, chest pain, or dyspnea. Infrequently, nodules can burst, causing pneumothorax (collapsed lung).
Airway Disease
RA can also cause inflammation and narrowing of the airways, resulting in bronchiectasis or small airway disease. Bronchiectasis is when the airways are abnormally and permanently widened, which means excess mucus can accumulate in them, resulting in recurring infections and constant coughing. In contrast, small airway disease originates in the smallest airways of the lungs and is associated with wheezing, breathlessness, or other asthma-like symptoms.
Pulmonary Hypertension
RA also has other complications like pulmonary hypertension, i.e., high blood pressure in the arteries of the lungs. This occurs when the blood vessels in the lung are damaged, resulting in decreased ability of blood to flow through them. Eventually, this added pressure can cause the heart to wear out and fail. Pulmonary hypertension symptoms include shortness of breath, fatigue, chest pain, and fainting.
Diagnosis of Lung Involvement in patients with RA
Timely recognition of lung complications is essential for treating their progression and outcomes. Pulmonary involvement in RA may be diagnosed using a combination of tools by physicians, including:
Imaging—Chest X-rays and high-resolution computed tomography (HRCT) scans are crucial in visualizing changes in lung tissue, including scarring, nodules, or fluid accumulation.
Pulmonary Function Tests (PFTs): ** These identify lung size and how well you can move oxygen, useful in diagnosing ILD or airway disease
Bronchoscopy commonly refers to a procedure where a thin, flexible tube is inserted into the airways to collect samples or visualize lung tissue directly.
— Biopsy: A lung biopsy may be required to confirm the diagnosis and establish how much lung tissue is affected.
Treatment for RA-Related Lung Problems
Effective management of pulmonary complications in the setting of RA requires a collaborative approach between rheumatologists, pulmonologists, and other specialists. The goal of treatment is to reduce inflammation, slow the progression of disease, and manage symptoms.
Medications
Corticosteroids: They are commonly prescribed to ameliorate inflammation in situations such as pleuritis or acute flares of ILD.
Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs class radio for managing RA (e.g., methotrexate and biologics) can indirectly contribute to lung health by lowering systemic inflammatory status associated with RA.
Antifibrotic drugs: Newer antifibrotic medications (e.g., pirfenidone or nintedanib) may reduce the progression of scarring in the lungs for patients with ILD.
Bronchodilators and mucolytics—these drugs can help alleviate symptoms of airway disease by opening airways and expelling mucus.
Oxygen Therapy
People with the most advanced lung disease, or those who have low blood oxygen levels, may require supplemental oxygen to help them breathe and function more effectively, thus enhancing their quality of life.
Pulmonary Rehabilitation
The program integrates exercise, education, and support to help people with lung disease manage symptoms, become more active, and improve their quality of life.
Lung Transplantation
Lung transplantation may be performed in selected patients with severe RA-associated lung disease, particularly progressive ILD, where it is considered a last resort option.
Long-term Outcomes of Lung Involvement in RA
Although not all pulmonary complications may be preventable, certain strategies might help lower the risk or lessen their impact:
Do Not Smoke: Smoking highly predisposes RA patients to develop lung disease and is also known to aggravate existing conditions. Giving up smoking is one of the best ways to safeguard lung well-being.
This can include: routine monitoring: regular appointments with your doctor and, at some stage, pulmonary characteristic assessments.
Vaccinations: Influenza and pneumoccocal infections can worsen the lung problems; thus, these vaccines are available to avoid these infections
Meds:** Collaborating with a healthcare provider to ensure RA treatment is fully optimized will decrease systemic inflammation affecting the lungs.
Part 2: Ongoing Living with RA and Lung Disease
Dealing with RA and related lung issues can be difficult, but they can be managed well with support. By staying informed, keeping channels of communication open with providers, and being proactive in health behavior, quality of life can be enhanced while burden of disease can be reduced.
RA is a systemic disease, and although mostly it affects joints, involvement of the lungs also needs to be addressed during routine RA care. Research and treatment have come a long way, and many RA patients now have more ways than ever to address the health of both their joints and lungs.



Leave a Reply